History:A 17-year-old girl presents with proximal left arm pain for two months prior to presentation. Patient has no history of trauma.
Frontal radiograph of the left humerusis shown below.

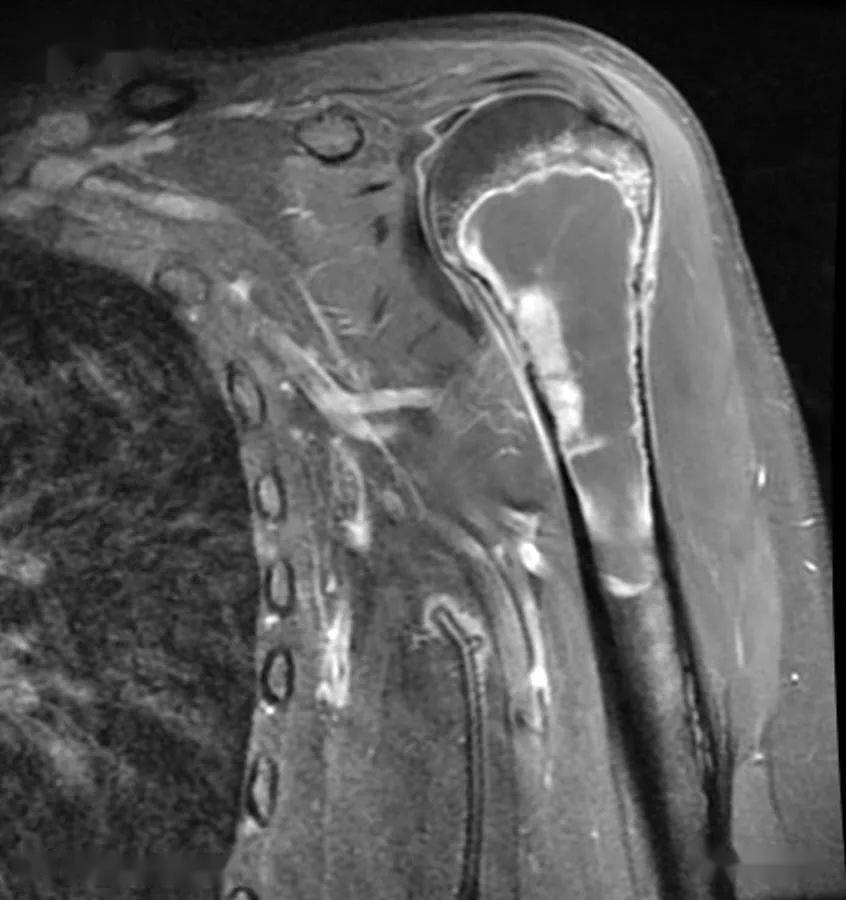
MRIwas attained for further evaluation.

Findings
- Radiograph: Frontal external rotation view of the left humerus demonstrates an expansile, lucent metaphyseal lesion with thin sclerotic rim and narrow zone of transition . There is cortical thinning without evidence of cortical break through or periosteal reaction. No calcified matrix is identified. No pathologic fracture is identified (including lack of “fallen fragment” sign associated with simple bone cysts).
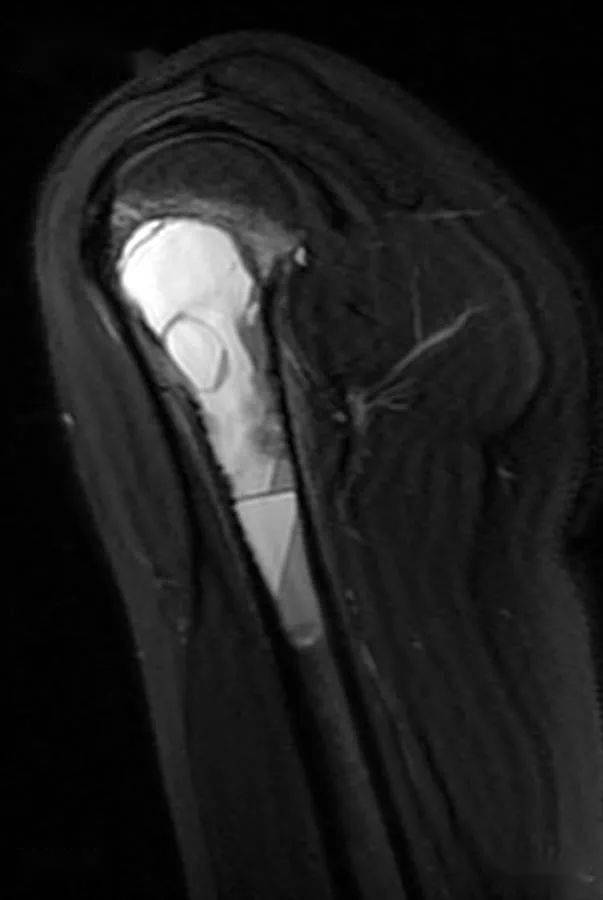
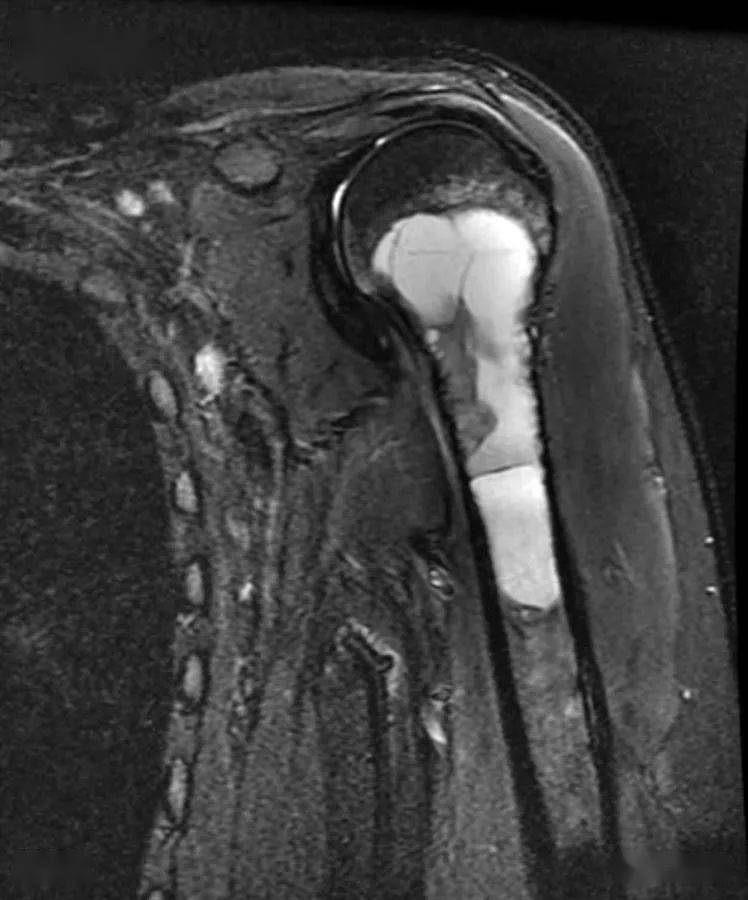
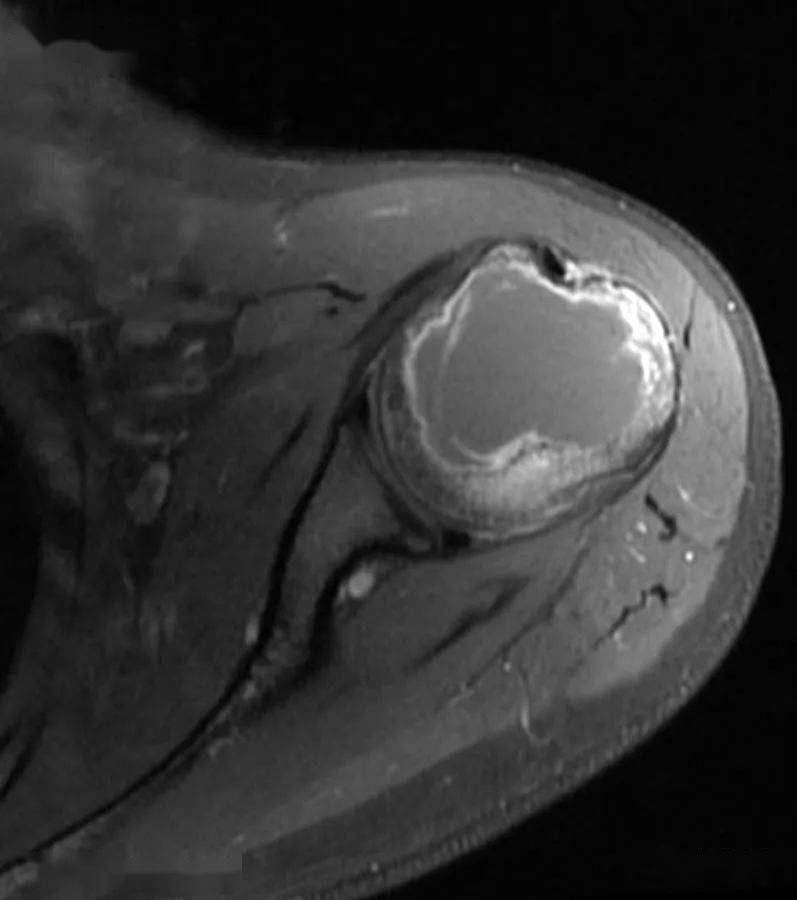
- MRI: MRI of the humerus demonstrates a multilocular, septated, expansile lesion in the proximal humeral metadiaphysis , corresponding to the lesion seen on radiograph. The associated cortical thinning is well-demonstrated on T1-weighted images. There are no areas of cortical breakthrough, significant periosteal reaction, or extension into the soft tissue. Mild reactive edema and enhancement is seen in the adjacent marrow. Multiple fluid levels, corresponding to layering blood products , are seen throughout the lesion, best depicted on T2 and short tau inversion-recovery (STIR) images. On postgadolinium images, there is thin rim and septal enhancement . There is also a small, eccentrically located enhancing, mildly T2 hyperintense solid component (best depicted on coronal T1 postgadolinium image), corresponding to reactive granulomatous tissue, which can be seen in this type of lesion. The majority of the lesion is cystic in composition.
Differential diagnosis
- Aneurysmal bone cyst
- Giant cell tumor
- Unicameral bone cyst
- Telangiectatic osteosarcoma
- Chondroblastoma
- Osteoblastoma
Diagnosis:Aneurysmal bone cyst
Key points
Aneurysmal bone cyst (ABC)
动脉瘤样骨囊肿
Pathophysiology
- Benign bone tumor, with the following components:
- Small solid components corresponding to granulomatous tissue, with the same cell composition as the septa
- Intervening connective tissue septa containing giant cells, osteoclasts, fibroblasts, and osteoblasts with reactive bone formation
- Blood-filled cystic spaces
- Etiology:
- Small solid components corresponding to granulomatous tissue, with the same cell composition as the septa
- Intervening connective tissue septa containing giant cells, osteoclasts, fibroblasts, and osteoblasts with reactive bone formation
- Blood-filled cystic spaces
- Primary (majority of cases): De novo formation; etiology remains controversial.
- Primary (majority of cases): De novo formation; etiology remains controversial.
- Proposed mechanism includes primary neoplastic physiology or development following vascular insult, such as venous obstruction.
- Proposed mechanism includes primary neoplastic physiology or development following vascular insult, such as venous obstruction.
- Proposed mechanism includes primary neoplastic physiology or development following vascular insult, such as venous obstruction.
- Secondary: Associated with other pre-existing osseous neoplasms (identified in approximately 30% of cases).
- Giant cell tumor (most common)
- Osteoblastoma
- Chondroblastoma
- Fibrous dysplasia
- Primary bone malignancies such as osteosarcoma and chondrosarcoma
- Genetics: Associated with abnormalities on chromosome 17.
- Secondary: Associated with other pre-existing osseous neoplasms (identified in approximately 30% of cases).
- Giant cell tumor (most common)
- Osteoblastoma
- Chondroblastoma
- Fibrous dysplasia
- Primary bone malignancies such as osteosarcoma and chondrosarcoma
- Genetics: Associated with abnormalities on chromosome 17.
- Giant cell tumor (most common)
- Osteoblastoma
- Chondroblastoma
- Fibrous dysplasia
- Primary bone malignancies such as osteosarcoma and chondrosarcoma
- Location:
- Long bones in majority (70% to 80%) of cases, with predilection for femur, tibia, and humerus
- Vertebrae in 15% of cases, with predilection for posterior elements
- Long bones in majority (70% to 80%) of cases, with predilection for femur, tibia, and humerus
- Vertebrae in 15% of cases, with predilection for posterior elements
- Natural history:
- Phases of cyst growth on radiography:
- Phases of cyst growth on radiography:
- 1: Small lucent lesion; no periosteal lifting.
- 2: Rapid enlargement, fusiform expansile changes, “blowout” appearance.
- 3: Growth slows/stops or intervention occurs.
- 4: Healing occurs with progressive calcification/ossification of the cyst cavity.
- 1: Small lucent lesion; no periosteal lifting.
- 2: Rapid enlargement, fusiform expansile changes, “blowout” appearance.
- 3: Growth slows/stops or intervention occurs.
- 4: Healing occurs with progressive calcification/ossification of the cyst cavity.
- 1: Small lucent lesion; no periosteal lifting.
- 2: Rapid enlargement, fusiform expansile changes, “blowout” appearance.
- 3: Growth slows/stops or intervention occurs.
- 4: Healing occurs with progressive calcification/ossification of the cyst cavity.
- Pathologic fracture: Most commonly in the vertebrae; can lead to vertebra plana.
- Following curettage, there is a moderate rate of recurrence (20% to 50% in reported series).
- Malignant transformation has been reported in a small number of cases.
- Controversial whether it truly occurs or not given the possibility of missing a pre-existing malignancy in setting of secondary aneurysmal bone cyst.
- Signs of malignancy (such as telangiectatic osteosarcoma) include cortical breakthrough, soft-tissue component, and wide zone of transition.
- Pathologic fracture: Most commonly in the vertebrae; can lead to vertebra plana.
- Following curettage, there is a moderate rate of recurrence (20% to 50% in reported series).
- Malignant transformation has been reported in a small number of cases.
- Controversial whether it truly occurs or not given the possibility of missing a pre-existing malignancy in setting of secondary aneurysmal bone cyst.
- Signs of malignancy (such as telangiectatic osteosarcoma) include cortical breakthrough, soft-tissue component, and wide zone of transition.
- Controversial whether it truly occurs or not given the possibility of missing a pre-existing malignancy in setting of secondary aneurysmal bone cyst.
- Signs of malignancy (such as telangiectatic osteosarcoma) include cortical breakthrough, soft-tissue component, and wide zone of transition.
Epidemiology
- Aneurysmal bone cysts encompass 2% to 9% of primary bone neoplasms.
- There is a wide age range at diagnosis, but the majority of patients are younger than 20 years old (median age: 13 years).
- There is no gender predilection.
Clinical presentation
- Edema, pain at site of cyst
- Pathologic fracture, most commonly associated with vertebral aneurysmal bone cyst
Imaging features
- Radiography:
- Lucent lesion with variable presence of visible internal trabeculations
- Narrow zone of transition with thin sclerotic margin
- Metaphyseal location, eccentric position (with growth, lesions can become central)
- Expansion of involved bone with growth (refer to phases described in the natural history section)
- Characteristic “soap bubble” appearance, referring to thinning of the cortex and elevation of the periosteum, with associated trabeculation
- Lucent lesion with variable presence of visible internal trabeculations
- Narrow zone of transition with thin sclerotic margin
- Metaphyseal location, eccentric position (with growth, lesions can become central)
- Expansion of involved bone with growth (refer to phases described in the natural history section)
- Characteristic “soap bubble” appearance, referring to thinning of the cortex and elevation of the periosteum, with associated trabeculation
- MRI:
- Cystic components encompass the majority of the lesion.
- Cystic components encompass the majority of the lesion.
- Varying signal intensity due to varying age of blood products; layering blood products produce characteristic fluid levels on imaging.
- No enhancement.
- Varying signal intensity due to varying age of blood products; layering blood products produce characteristic fluid levels on imaging.
- No enhancement.
- Varying signal intensity due to varying age of blood products; layering blood products produce characteristic fluid levels on imaging.
- No enhancement.
- Intervening septa: enhancing
- Solid components:
- T1 isointense to muscle
- T2 hyperintense
- Enhancing
- Reactive edema in the adjacent bone and soft tissue
- Intervening septa: enhancing
- Solid components:
- T1 isointense to muscle
- T2 hyperintense
- Enhancing
- Reactive edema in the adjacent bone and soft tissue
- T1 isointense to muscle
- T2 hyperintense
- Enhancing
Differential diagnoses
- Giant cell tumor
- Unicameral bone cyst
- Telangiectatic osteosarcoma
- Chondroblastoma
- Osteoblastoma
Treatment
- Surgery is the mainstay.
- Curettage and bone grafting.
- Adjuvant cryotherapy and sclerotherapy can be applied during curettage to reduce recurrence.
- Radiation is used in cases with unresectable or subtotally resected lesions.
- Recurrence can occur in up to half of cases, particularly with lesions adjacent to the physis.
- Curettage and bone grafting.
- Adjuvant cryotherapy and sclerotherapy can be applied during curettage to reduce recurrence.
References
- Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: Unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res. 2015;101(1 suppl):S119-S127.
- Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP. Aneurysmal bone cyst. Am J Clin Oncol. 2006;29(3):311-315.